ORIGINAL ARTICLE | https://doi.org/10.5005/jp-journals-10006-1742 |
Management of Pelvic Abscess—Challenges for a Gynecologist
1,2Department of Obstetrics and Gynaecology, Ramaiah Medical College, Bengaluru, Karnataka, India
Corresponding Author: Anirudha R Podder, Department of Obstetrics and Gynaecology, Ramaiah Medical College, Bengaluru, Karnataka, India, Phone: +91 9845130055, e-mail: arpodder@gmail.com
How to cite this article Podder AR, Seshadri JG. Management of Pelvic Abscess—Challenges for a Gynecologist. J South Asian Feder Obst Gynae 2020;12(1):10–17.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Objectives: To analyze the difficulties in diagnosis, treatment, and postoperative care in patients with pelvic abscess.
Study design: This is an observational study; 11 patients underwent laparotomy for drainage of pelvic abscess between January 1, 2015, and December 31, 2018. The diagnosis of pelvic abscess was a spot diagnosis only in one patient. It was a surprise finding, on table, in three patients. The most common confounding diagnosis was ovarian torsion. Two patients had subacute intestinal obstruction like clinical features.
Results: All patients improved following laparotomy and drainage of pus. In the first six patients in our series, the skin was closed immediately following closure of the rectus sheath, and all of them developed wound dehiscence. In the last five patients in our series, delayed primary closure was performed. The skin was closed after wound turned healthy and comorbid conditions controlled and corrected. All five patients had a healthy scar. The shortest duration of hospital stay was 18 days, and the longest duration of hospital stay was 55 days.
Conclusion: Pelvic abscess is one condition which can test the clinical acumen of a gynecologist to make a prompt and correct diagnosis and to manage multiple postoperative problems like uncontrolled diabetes, sepsis, and a wound which will require daily dressing for several days. This is one of the few gynecological conditions where a delayed primary closure should be performed. And most importantly, the gynecologist has to manage spiraling treatment costs and a falling patient morale.
Keywords: Delayed primary closure, Pelvic abscess, Pus, Re-suturing, Wound dehiscence..
INTRODUCTION
Most of the surgical emergencies faced by an obstetrician gynecologist today are obstetrical in nature. Pelvic abscess which usually presents as pain abdomen is less frequently encountered and can thus be a diagnostic dilemma and a challenging condition to treat. Pelvic abscess is a severe form of acute pelvic inflammatory disease.1 Sexual promiscuity, diabetes mellitus, and lack of asepsis while performing uterine evacuation are the known causes of pelvic abscess.1 Increased awareness about sexually transmitted diseases and diabetes and improved health care have made pelvic abscess a less commonly encountered gynecological emergency. However, when a gynecologist does encounter one such case, it can indeed turn out to be a frustrating experience for both doctor and patient.
OBJECTIVES
To analyze the difficulties in diagnosis, treatment, and postoperative care in patients with pelvic abscess.
STUDY DESIGN
This is an observational study; 11 patients underwent laparotomy for drainage of pelvic abscess between January 1, 2015 and December 31, 2018. All patients were assessed, operated, and managed postoperatively by the corresponding author. An emergency laparotomy was performed in 10 patients, and 1 patient underwent an elective laparotomy.
Four patients were obese diabetics with one patient also having rheumatic heart disease (RHD) with mitral stenosis and regurgitation.
Three patients were puerperae, with a history of emergency cesarean delivery less than a fortnight back.
In three patients, the diagnosis of pelvic abscess was a complete surprise, detected on table after the peritoneum was opened. All three were suspected to have an ovarian tumor, with acute torsion suspected in two patients; in one patient among these two, diabetes mellitus was detected for the first time, postoperatively.
And finally, one patient was a recently confirmed case of carcinoma cervix IIIB and was to start chemoradiation.
The diagnosis of pelvic abscess was a spot diagnosis only in one patient who came with acute pain abdomen and foul smelling copious discharge from lower segment cesarean section (LSCS) wound.
The most common confounding diagnosis was ovarian torsion which was suspected initially in five patients. Two patients had subacute intestinal obstruction like clinical features. The detailed profile of all patients is mentioned in Table 1.
RESULTS
All patients improved following laparotomy and drainage of pus. In the first six patients in our series, the skin was closed immediately following closure of the rectus sheath with a suction drain in the subcutaneous space. All six patients developed wound dehiscence. Daily dressing with eusol and povidone iodine pack was done till the wound turned healthy. The wound was re-sutured under anesthesia after anemia, and hypoproteinemia were corrected and sugars controlled in diabetics. Four patients had a healthy scar following re-suturing. One patient developed partial wound gape after re-suturing and underwent repeat re-suturing under local anesthesia. The sixth patient returned a month after discharge with a nonhealing wound which was managed by debridement and vacuum-assisted closure in conjunction with plastic surgeons.
| S. no. | Patient profile | Examination findings | Investigations | Imaging findings |
|---|---|---|---|---|
| Known diabetics | ||||
| All were multiparous, obese, and had poor glycemic control. All had pain and tenderness and no appreciable mass on internal examination | ||||
| 1 |
|
| Total count: 16,200/mm3 | USG done outside: 54 × 35 × 56 mm solid cystic mass in left adnexa Collection 90 × 30 × 105 mm with internal echoes CT scan done outside by the referring doctor: left tubo-ovarian abscess |
| 2 |
|
| Total counts: 27,100/mm3 CA-125: 23.6 IU/mL | Emergency USG: 15.9 × 4.2 cm left adnexal mass, moderate ascites, edematous bowel loops |
| 3 |
|
Was seen as an outpatient and was asked to follow-up with reports, presented with acute abdomen in the casualty next evening | Total count: 13,430/mm3 CA-125: 74 IU/mL | USG done outside: bilateral multi-loculated cystic lesions measuring 4.4 × 3.6 cm in right and 4.8 × 3.8 cm in left Repeat USG at our hospital shows normal study with minimal free fluid |
| 4 |
|
| Total count: 38,570/mm3 | CT scan done outside 10 days before patient presented to our institute showed thick walled solid cystic lesion with septations in the left adnexa 10 × 8.5 cm, left ovary not seen separately Impression: complex ovarian cyst with partial torsion Emergency USG at our institute: complex left ovarian cyst 75 × 63 mm or torsion, minimal ascites |
| Puerpera | ||||
| All had had a cesarean delivery recently and the LSCS wound had gaped. All had a sub-involuting uterus, tenderness, but no appreciable mass on examination | ||||
| 5 |
|
| Total count: 32,640/mm3 Bilirubin: 3.6 mg%, creatinine: 1.8 mg% APTT: 102 s Procalcitonin: 70.5 Total count after 6 days: 20,110/mm3 LFT and RFT normal |
CT-guided aspiration showed yellow turbid fluid, fluid analysis showed leukocytosis |
| 6 |
|
| Total count: 24,112/mm3 | USG not done Diagnosis of abscess obvious Immediately taken for laparotomy |
| 7 |
|
| Total count: 13,560/mm3, this patient was on antibiotics since delivery | CECT: moderate ascites Taken for laparotomy on day 6 of admission when no improvement was noted |
| Suspected ovarian tumor | ||||
| 8 |
|
| Total count: 39,330/mm3 CA-125: 219.2 IU/mL Total count: 17,160/mm3 | Emergency USG: right ovarian cyst or torsion |
| 9 |
|
| CA-125: not done taken up for laparotomy immediately for suspected ovarian torsion FBS was normal | USG done outside: 55 × 59 × 70 mm mass not seen separately from left ovary CT scan: 83 × 72 mm in left adnexa, another mass 68 × 42 mm mass in the pouch of Douglas |
| 10 |
|
| Total count: 7,640/mm3 Platelet count: 9.2 lakhs/mm3 CA-125: 115 IU/mL AFP, LDH, β-hCG: all normal | MRI: two cystic lesions: 10.3 × 5.5 × 6.7 cm, abutting rectum, and 10.2 × 5.4 × 8.8 cm anterior to rectum, right hydroureteronephrosis |
| 11 |
|
|
| CECT: likely tubo-ovarian abscess and pelvic collection with small pockets of air |
USG, ultrasonography; CA, cancer antigen; MS, mitral stenosis; MR, mitral regurgitation; EF, ejection fraction; POD, pouch of Douglas; CECT, contrast-enhanced computed tomography; APTT, activated plasma thromboplastin time; LFT, liver function test; RFT, rental function test; AFP, alpha fetoprotein; LDH, lactic dehydrogenase; FBS, fasting blood sugar; UTI, urinary tract infection
In the last five patients, delayed primary closure was performed, all of which healed well.
All 11 patients recovered after a protracted course, with 1 patient requiring a second admission for 20 days for a nonhealing wound. The shortest duration of hospital stay was 18 days, and the longest duration of hospital stay was 55 days.
DISCUSSION
When managing a case of pelvic abscess, the first challenge for a gynecologist is to make the correct diagnosis. The differential diagnosis of pelvic abscess includes ovarian torsion, ectopic pregnancy, acute appendicitis, and diverticulosis.2,3 Almost all patients present with acute/acute on chronic abdomen, and the gynecologist first has to exclude non-gynecological causes or, in other words, has to confirm the gynecological nature of abdominal pain. This is often easier said than done because the diagnosis of pelvic abscess can be a dilemma, since it is not a common condition.
To highlight this point, we would like to point out that more than 2,000 deliveries are conducted, and more than 800 gynecological procedures are performed every year at our institute. Emergency cesarean section is the most common emergency laparotomy performed, while ectopic pregnancy is the commonest gynecological cause of acute abdomen. During the above period, more than 100 cases of ectopic pregnancy were encountered, out of which 64 surgeries were performed which include emergency laparotomy for ruptured ectopic and laparoscopic salpingectomy. The rest were managed conservatively. The diagnosis of ectopic pregnancy has become easy with the availability of ultrasound and β-human chorionic gonadotropin (β-hCG) titers.
On the contrary, the other causes of acute abdomen, i.e., ovarian torsion, pelvic abscess, severe dysmenorrhea, ovulation pain, etc., between January 1, 2015, and December 31, 2018, were less than 50 in number.
In a case of ovarian torsion, the gynecologist may be inclined to perform the surgery (which in most cases can be done laparoscopically) during routine hours, with good bowel preparation and when frozen section is available. This would obviate the need for a second surgery for restaging. However, a delay of this sort can be dangerous in case of pelvic abscess. Pus and flimsy adhesions between bowel loops start getting organized, making drainage and release of adhesions more difficult and making bowels more prone to injury. In case of diabetics, glycemic control is impossible till the pus is drained, and diabetics are more prone to develop septicemia.4
In our experience, the diagnosis of pelvic abscess should be a clinical one. Imaging is prone to subjective variation and should be correlated clinically. In our study, imaging was done by the radiologist on duty, and some patients were referred with an imaging report. The imaging report was helpful in preoperative diagnosis of pelvic abscess only in four patients, and in six patients, imaging was suggestive of an adnexal mass or torsion (Table 1).
Ultrasound is usually the first imaging modality because of its availability and affordability. The diagnosis of pelvic abscess is based on the fact that the normal diameter of the fallopian tube should not be more than 4 mm, and the presence of a visible fallopian tube is suspicious.5 Finding a thick fallopian tube with echogenic wall due to edema is suggestive though nonspecific. The contents of the tube could be anechoic or echogenic—which is suggestive of pus.5 The presence of air-fluid levels is pathognomonic of pyosalpinx. Oophoritis is seen as increase in ovarian size with loss of corticomedulary differentiation. If ovarian involvement is such that fallopian tube and ovary can no longer be identified separately, then one has to consider a differential diagnosis of ovarian tumor.5 An error on either side can be deleterious since it can either result in a surgery done without adequate preparation or a delay that could be life-threatening.
Computed tomography (CT) scan is superior to differentiate whether the inflammation is gynecological, gastrointestinal, or urological in nature. Magnetic resonance imaging (MRI) is superior to CT scan when one needs to distinguish between tubo-ovarian abscess and an ovarian tumor, and unlike CT scan be done in pregnant women.5 However, the signs of inflammation are relatively nonspecific. Endometritis is seen as enlargement of endometrial cavity, and tubal involvement is seen as enlargement in the form of serpentine structures. Ovarian involvement is seen as ovarian enlargement with multicystic ovary or as an actual adnexal mass with hypodense thick walls, which is also suspicious of an ovarian tumor.5
The presence of air-fluid levels which is pathognomonic of pus is seen in only about 22–38% of cases. And when this sign is not present, it is difficult to distinguish pus from other body fluids on imaging.5
A comparison between presenting features of patients with pelvic abscess and those cases with ovarian torsion assessed and managed by the authors shows that tachycardia can be present in both, though not necessarily (Table 2). The single most important sign is the presence of tenderness on abdominal and vaginal examination, but clinically no demonstrable mass, in cases of pelvic abscess. There can, at the most, be a boggy fullness in the adnexa and/or the pouch of Douglas.
But in case of ovarian torsion, there will always be a palpable mass, which can be appreciated despite extreme tenderness. Even in obese women and women with a small adnexal mass, in whom no mass can be felt abdominally, a firm mass in the fornix and/or the pouch of Douglas can be well appreciated.
Mild leukocytosis may or may not be present in ovarian torsion, but significant leukocytosis is almost always present in case of pelvic abscess, unless inappropriate antibiotic treatment has been given.2
| Pelvic abscess | Ovarian torsion |
|---|---|
| Usually presents as acute or acute on chronic abdomen | Can present as acute abdomen or chronic abdomen or intermittent pain abdomen with periods of worsening and partial improvement due to partial twisting and untwisting of ovarian tumor |
|
|
|
|
| The above signs may be masked by inappropriate antibiotic treatment, the history of which patient may or may not give | There is a firm mass that can be appreciated on abdominal examination depending on size and always on pelvic examination despite tenderness and coexisting obesity |
| On examination, there is significant tenderness but no appreciable mass. There might be fullness or bogginess in the fornices and/or the pouch of Douglas | Ultrasound is reliable and can correctly detect an ovarian tumor |
| Ultrasound is less useful though it can detect other coexisting pathology, like hernia etc. Tenderness and bowel gas shadows make ultrasound diagnosis difficult | |
| CT and MRI might be more useful |
All our patients were managed by surgical drainage of pus. Although ultrasound- and CT-guided aspiration of pus have been described, it depends on the availability of intervention radiologist and an accurate diagnosis of pelvic abscess by imaging. It is futile when the diagnosis is uncertain or when facilities are not available. Our own experience shows the limited utility of imaging in both diagnosis and treatment of pelvic abscess. Culdocentesis can be done to obtain a sample of fluid from the pouch of Douglas; the presence of pus confirms the presence of an abscess. Colpotomy can then be performed to drain the pus. However, in hindsight, all our patients had bowel loops agglutinated to one another and to the uterus. Culdocentesis and colpotomy can at the most confirm the presence of pus in the pouch of Douglas but not when pus is present elsewhere in the abdominopelvic cavity, neither can bowel adhesions be released through a colpotomy. Also, colpotomy is not without risks of injury to visceral organs.6 In our experience, conservative treatment should not be attempted; drainage should be the rule.7,8
A vertical incision (Fig. 1) extending from symphysis pubis to a little above the umbilicus was taken in all patients. Thus, our puerperal patients, who had undergone a cesarean delivery a few days before, ended up having an inverted T scar on the abdomen.
Laparoscopy was attempted only in one patient, in our series. This was in a young lady with a firm mass in left adnexa with suspected ovarian tumor but was converted into a laparotomy when dense adhesions between bowel loops were encountered. This was our only patient who underwent an elective procedure. This patient gave a history of multiple courses of antibiotics for her abdominal pain and the abscess had organized to become an “antibioma.”
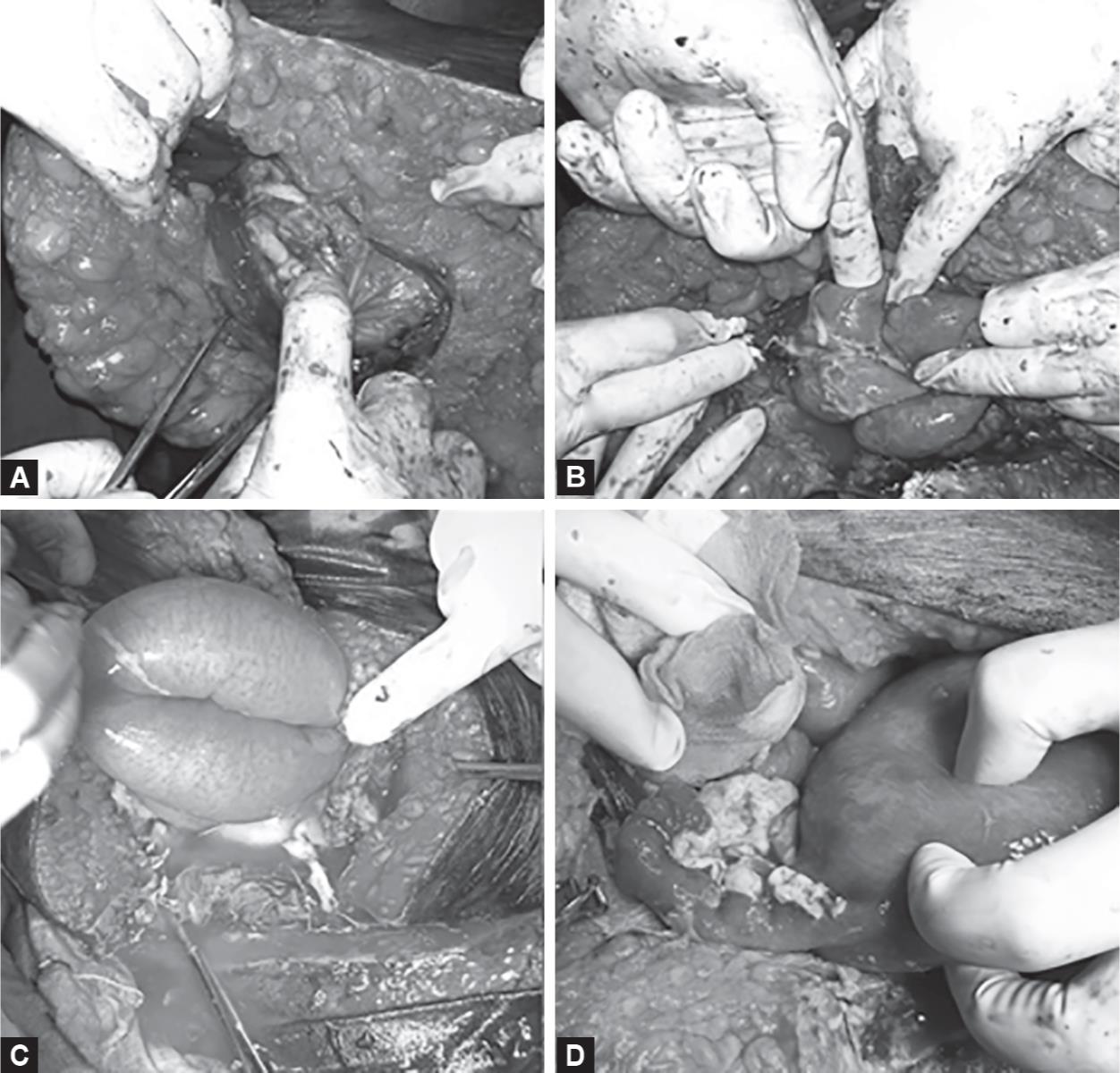
Figs 1A to D: (A) Presence of pus on opening the peritoneum and the care with which the peritoneum needs to be incised; (B) Bowel loops agglutinated to each other due to flimsy adhesions; (C) Dilated proximal jejunum of the patient who presented with sepsis and was taken up with suspected subactute intestinal obstruction; (D) Purulent flakes present on the posterior surface of uterus and adnexa. Figures A, B, and D are of patient 4. The obese nature of the abdomen can be appreciated. Figure C is of patient 5. The transverse LSCS wound and the fact that the abdomen is not obese can be appreciated
In our experience, laparoscopy would not be advisable since all our patients had dilated, edematous bowel loops agglutinated to each other and to the anterior peritoneum by flimsy adhesions (Fig. 1). The omentum had localized the pus, rightfully called the “Policeman of the abdomen”, and it had to be released to break the septations and drain the collection. In some patients, a loop of bowel had formed the part of the abscess wall and had to be separated, very carefully. Pus samples were taken for culture and sensitivity as soon as it was seen pouring out (Fig. 2). After the pus was drained, the abdomen and pelvis were thoroughly irrigated with copious amounts of saline, small bowel traced from duodenojejunal flexure to ileocecal junction to check for any injury and mesenteric rents. Cecum, sigmoid, and rectum were also checked for injuries. Necrotic tissue was gently peeled out, leaving the uterus and other tissues in place. Fallopian tubes and ovaries were badly damaged and were not recognizable in some patients (Fig. 2). Abdomen was closed with drains placed in the pouch of Douglas.
Postoperatively, all patients were managed in the intensive care unit (ICU), for correction of anemia and control of blood sugars. All of them improved gradually. One of our diabetic patients had to be reexplored on day 5 because frank pus reappeared in the drain. Attempts at colpotomy failed. On reexploration, it was found that the first exploration had been performed hurriedly, and some locules were still intact.
Culture yielded Escherichia coli in five patients and Staphylococcus aureus in two patients. Those patients who had received antibiotics preoperatively had no organisms grown on culture.
None of the patients were tested positive for human immunodeficiency virus. Since all of them improved following drainage of pus, and since the cause of pelvic abscess appeared to be ascending infection due to sexual transmission, uncontrolled diabetes, or secondary infection of cervical malignancy, there was no indication to evaluate any of the patients further for other possible causes like tuberculosis.
The first six patients in our series developed a full-length gape (Fig. 3). We had closed the abdomen in layers with drains placed in the pouch of Douglas and subcutaneous space. The wound gape was managed by daily dressing with eusol and povidone iodine pack till healthy granulation tissue was present all over. Re-suturing was done under spinal anesthesia. Four patients had a healthy wound following re-suturing. One patient had a partial wound gape following re-suturing which was sutured under local anesthesia (Fig. 3). One obese diabetic patient returned a month after re-suturing with a nonhealing wound which was managed by debridement and vacuum-assisted closure in conjunction with plastic surgeons (Fig. 4).

Figs 2A to C: (A) Purulent flakes present on the undersurface of liver, and this image is of patient 7; (B) Pus pouring out after septations have been broken; (C) Pus being released from uterine fundus and adnexa which have turned necrotic and are not recognizable. Figures B and C are of patient 4
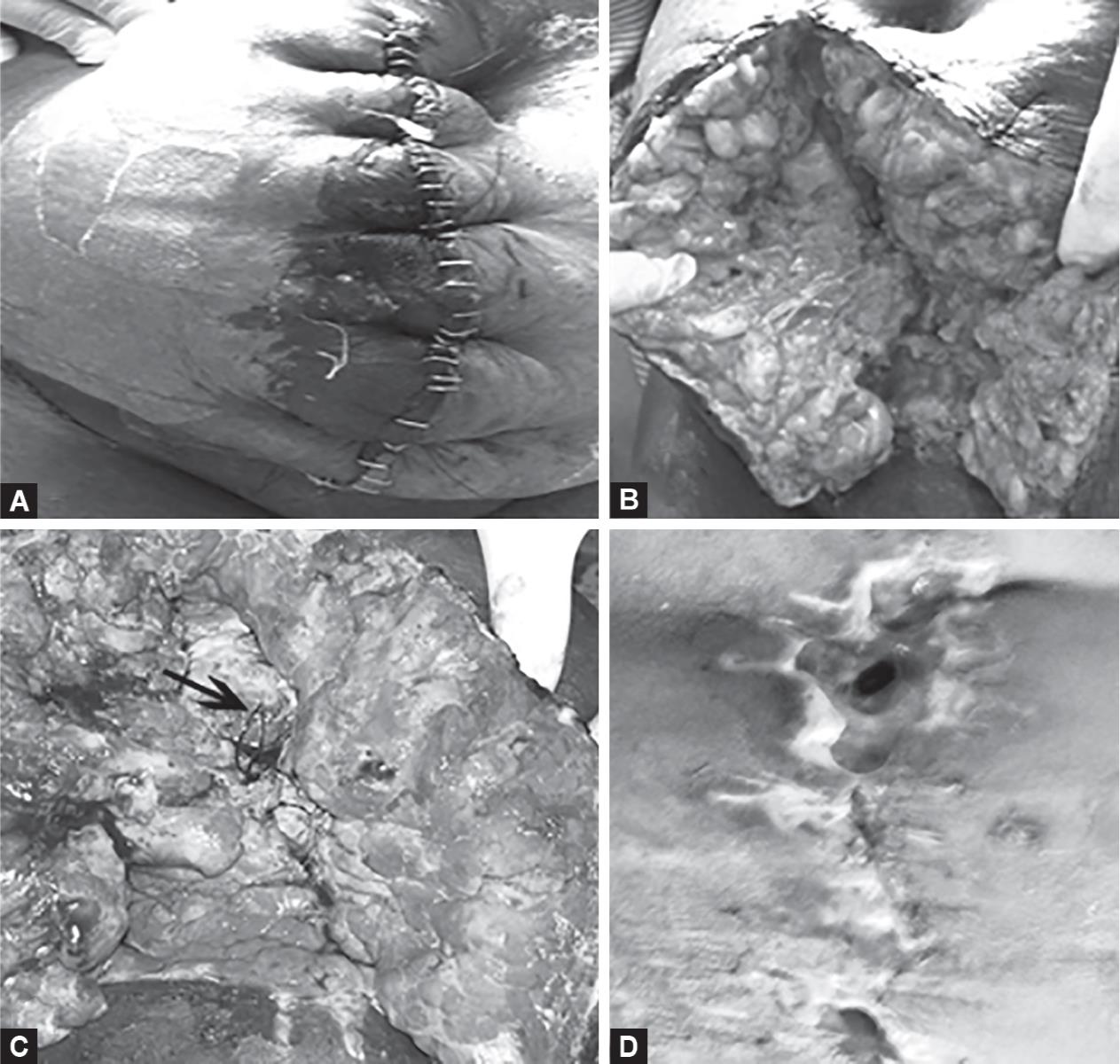
Figs 3A to D: (A) Primary closure of the skin showing obvious infection; (B) Complete wound dehiscence with pale poorly vascularized adipose tissue, and the suffering due to the long delay in wound healing can be appreciated. This patient returned later with a chronic nonhealing wound; (C) The same wound after 7 days of daily dressing with eusol and povidone iodine showing improved blood supply, but the defect in rectus sheath can be appreciated. Figures A to C are of patient 4; (D) Partial wound gape following re-suturing showing a larger defect in the upper end at the level of umbilicus and a smaller defect at the lower end. Figure D is of patient 3, a known diabetic and a known case of RHD with mitral stenosis and regurgitation

Figs 4A to E: (A) A nonhealing wound where the tunnel beneath the skin can be appreciated; (B) The same wound closed following debridement using vacuum-assisted closure. Figures A and B are of patient 4; (C) Delayed primary closure where the skin is packed with povidone iodine gauze after closure of rectus sheath and one can appreciate there are no suture marks on the skin edges; (D) The same wound after 5 days showing pale adipose tissue; (E) The same wound just before closure showing healthy granulation tissue. Figures C to E are of patient 5
Wound dehiscence is an inevitable complication following immediate closure of a contaminated wound. It is one of the main reasons for prolonged stay and increased costs. We adopted delayed primary closure in the last five patients of our series, after our disappointing experience with primary closure. Delayed primary closure of the abdominal wound was widely practiced for warfare wounds during World War I before the advent of antibiotics.9 This technique involves closure of the rectus sheath of abdomen and packing the subcutaneous space with gauze soaked in povidone iodine. The wound is dressed daily, and the skin is closed after the fifth postoperative day when the blood supply to the skin edges has improved (Fig. 4). This technique is said to prevent wound dehiscence and reduce hospital stay, though the risk of hernia remains.10,11 However, in our experience, this need not be universal. Closure of skin can be done only after the patient has come out of sepsis and after correction of comorbid conditions like diabetes, anemia, and hypoproteinemia, and this period can vary from patient to patient. One of our patients who was in sepsis and whose closure was done by this technique developed supraventricular tachycardia postoperatively and had to remain in ICU for 22 days. The main advantage of delayed primary closure is that the “complication” of dehiscence and the associated disappointment is avoided for both patient and doctor.
Pelvic abscess is probably the only conditions where a gynecologist encounters a contaminated abdominal wound and closure by a delayed primary closure is recommended. Delayed primary closure should not be confused with open abdomen. Open abdomen is a defect created intentionally by not closing the incision after completion of surgery, or the abdomen is opened or reopened out of concern that the patient is developing abdominal compartment syndrome.
All our patients were discharged after a protracted course in good health. All of them were counseled about the high possibility that they may need to undergo more surgeries in future for incisional hernia, intestinal obstruction due to postoperative adhesions,12 recurrent abscess, and need for hysterectomy with salpingo-oophorectomy due to chronic pelvic inflammatory disease (PID). Diabetics were counseled about the dangers of poor glycemic control.
CONCLUSION
Pelvic abscess is not a commonly encountered emergency for a present-day gynecologist. Asian countries have a huge diabetic population.13 Despite improvements, there is still a lack of adequate health-care facilities and health awareness. And therefore, pelvic abscess will not become an unheard condition anytime soon. This is one condition which can test the clinical acumen of a gynecologist to make a prompt and correct diagnosis. This is one of the few conditions for a gynecologist where delayed primary closure of the abdomen can be followed since wound dehiscence is inevitable following primary closure. It also involves managing multiple postoperative problems like uncontrolled diabetes, sepsis, daily wound dressing for several days, spiraling treatment costs, and, most importantly, managing a falling patient morale.
ETHICAL STANDARDS
This article does not contain any studies with human participants or animals performed by any of the authors. All patients were managed as and when they presented to us and according to their clinical condition. A written informed consent for the procedure(s) performed was taken for all patients and a copy of it is in the case file of respective patients.
REFERENCES
1. Mitchell C, Prabhu M. Pelvic inflammatory disease: current concepts in pathogenesis, diagnosis and treatment, infectious disease clinics of North America. Infect Dis Clin North Am 2013;27(4):793–809. DOI: 10.1016/j.idc.2013.08.004.
2. Chappel CA, Weisenfeld HC. Pathogenesis, diagnosis, and management of severe pelvic inflammatory disease and tuboovarian abscess. Clin Obstet Gynecol 2012;55(4):893–903. DOI: 10.1097/GRF.0b013e3182714681.
3. Sato K, Kajihara T, Miki A, et al. Differential diagnosis of pelvic cystic lesions caused by hemorrhage from inflammatory abscess using CT attenuation in women with acute abdomen. Nagoya J Med Sci 2015;77(4):563–569.
4. Hirasawa H, Oda S, Nakamura M. Blood glucose control in patients with severe sepsis and septic shock. World J Gastroenterol 2009;15(33):4132–4136. DOI: 10.3748/wjg.15.4132.
5. Thomassin-Naggaraa I, Darai E, Bazota M. Gynecological pelvic infection: what is the role of imaging? Diagn Interv Imaging 2012;93(6):491–499. DOI: 10.1016/j.diii.2012.04.002.
6. Aimakhu CO, Olayemi O, Odukogbe AA. Surgical management of pelvic abscess: laparotomy versus colpotomy. J Obstet Gynaecol 2003;23(1):71–72. DOI: 10.1080/0144361021000043317.
7. Oride A, Kanasaki H, Miyazaki K. Therapeutic process of gynecological pelvic abscess—retrospective review of 20 cases. Surgical Science 2013;4(03):202–209. DOI: 10.4236/ss.2013.43038.
8. Mathai M, Sanghvi H, Guidotti RJ, et al. Managing Complications in Pregnancy and Childbirth. A guide for midwives and doctors, Culdocentesis and Colpotomy, Section 3, Procedures, WHO International, Department of Reproductive Health and Research. World Health Organization; 2000.
9. Chiang RA, Chen SL, Tsai YC. Delayed primary closure versus primary closure for wound management in perforated appendicitis: a prospective randomized controlled trial. J Chin Med Assoc 2012;75(4):156–159. DOI: 10.1016/j.jcma.2012.02.013.
10. Verdam FJ, Dolmans DEJGJ, Loos MJ, et al. Delayed primary closure of the septic open abdomen with a dynamic closure system. World J Surg 2011;35(10):2348–2355. DOI: 10.1007/s00268-011-1210-8.
11. van’t Riet M, Steyerberg EW, Nellensteyn J, et al. Meta-analysis of techniques for closure of midline abdominal, incisions. Br J Surg 2002;89(11):1350–1356. DOI: 10.1046/j.1365-2168.2002.02258.x.
12. Sartelli M. A focus on intra-abdominal infections. World J Emerg Surg 2010;5(1):9. DOI: 10.1186/1749-7922-5-9.
13. Kaveeshwar SA, Cornwall J. The current state of diabetes mellitus in India. Australas Med J 2014;7(1):45–48. DOI: 10.4066/AMJ.2014.1979.
________________________
© The Author(s). 2020 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.